Grade 3 AC Separation Surgery or Not
There are approximately 50,000 AC joint separations that occur each year in the US and most of them will be treated non-surgically (initially). But is this really the right decision? There is truly no right or wrong answer because this is a very hotly controversial area of modern day orthopedic treatment. So hopefully this section will help you think this decision through and make the treatment choice that is really best for your situation.
First – Accurate Diagnosis of AC Joint Separation Grade

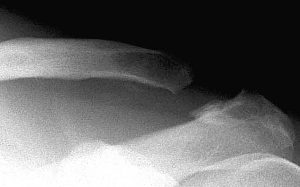
It is essential that your decision is based on accurate information, which means making sure you really do have a grade 3 AC joint separation. Unfortunately many patients are given this diagnosis without a proper evaluation and the information is simply incorrect. Many patients given a diagnosis of a grade 3 AC joint separation really have a more severe injury (Grade 5 especially), which requires surgery in most cases. This causes unnecessary delays in getting the best treatment and compromises the end result. So make sure your diagnosis is accurate. You must get an x-ray of both the normal and abnormal shoulder so that the separation can be measured accurately with digital x-ray technology. If the clavicle is more than twice the normal distance from the coracoid process (part of the scapula) then you really have a grade 5 ac joint separation, and not a grade 3.
Second
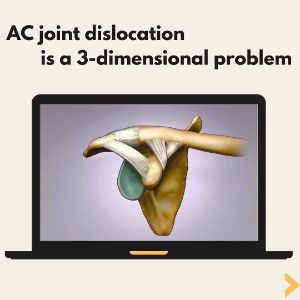
Once your ac joint injury has been accurately classified as a Grade 3 ac joint separation, the next thing to evaluate is horizontal stability. While the obvious problem in an AC joint injury is the vertical displacement of the clavicle it is clear from numerous recent research articles that an AC joint dislocation can cause significant abnormal movement in the horizontal plane. This can either be excessive posterior positioning of the clavicle or even in some cases excessive lateral positioning of the clavicle. A clavicle that has posterior position is a significant source of pain and when present foretells a poor prognosis for non-surgical treatment. More importantly, because the abnormality is in the plane of the x-ray, a standard x-ray cannot evaluate for horizontal instability. One way a patient can become aware of this is when the arm crosses in front of the body the clavicle which is already prominent becomes significantly more prominent. This can be evaluated with a special x-ray taken with the arm crossing in front of the body showing that the clavicle “overrides” the acromion underneath it. Some Grade 3 AC joint dislocations have horizontal instability and some do not. Knowing this allows the doctor to more accurately predict whether non-surgical treatment has much of a chance of success.
Non-surgical Option
This is a good consideration once you have been determined to have a horizontally stable true grade 3 AC joint dislocation. Whatever deformity exists, however, is permanent regardless of any mode of non-surgical treatment. For many patients, the “bump” deformity is unacceptable and surgery is the only way to address this. Approximately 50% of patients will make a full recovery without surgery and their return to sports will be much faster than going through surgical repair. About 25% of patients will have tolerable but low-grade ongoing symptoms that may affect athletic or work performance. This includes painful popping, clicking, and easy fatigability. Approximately 25% of patients will have high-grade residual symptoms and require surgery.
While it is often stated by orthopedic surgeons that only young or highly active patients should consider surgery, this has actually never been studied so if you are older than 35 you may be told that surgery is not a wise option. However, there is no evidence that older and less active patients fare any better with non-surgical treatment than younger patients so it is important to weigh the options carefully. The results from reliable reproducible procedures such as the Closed Loop Double Endobutton are 98% successful, so ultimately it’s a personal decision about weighing the uncertainty of non-surgical treatment with the commitment and extra recovery time of undergoing surgery.
AC Joint Surgery
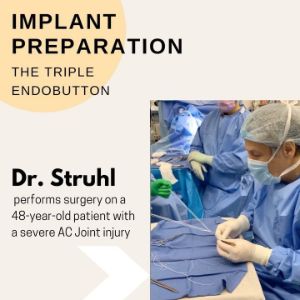
Surgery is the clear choice for highly displaced AC joint separations (Grade 4, 5, and 6), and also for Grade 3 AC separations that demonstrate significant horizontal instability. Deciding on a surgeon is critical to achieving a complication-free and pain-free result. Unfortunately, there is no “gold standard” procedure so different surgeons have different approaches. The failure / complication rate for most procedures is approximately 20-30% which is very discouraging. One popular technique involves using a “tendon graft” to stabilize the AC joint area. This requires using donor tissue (cadaver) to complete the procedure. Another popular option is an “arthroscopic” repair. This involves smaller incisions and is appealing because of the potential for less pain and quicker recovery. Both of these choices, however, have reported failure rates of 20-30% so it is important to choose your surgeon and the technique wisely!
There is another option for an AC joint surgery technique with better results backed by an 11-year clinical study being the Closed Loop Double Endobutton technique. The Closed Loop Double Endobutton technique, which Dr. Struhl uses exclusively, has been in use for over 15 years and has a proven success rate of 98%, with over 100 patients treated to date.